Virtual Reality for Medical Training: A Guide to Transforming Healthcare
Virtual reality for medical training provides healthcare professionals with a safe, repeatable, and fully immersive environment to master complex procedures without any risk to patients. It functions much like a flight simulator for pilots, but is designed for surgeons, nurses, and medical teams—a controlled, virtual world where they can perfect high-stakes skills long before entering a real clinical setting.
The New Frontier in Medical Education

For generations, medical education has followed a familiar path: textbooks, lectures, and hands-on practice with cadavers or, eventually, live patients. While foundational, these methods have inherent limitations. A textbook cannot convey the tactile sensation of a surgical instrument, and opportunities for hands-on practice are often limited, expensive, and carry inherent risks.
Virtual reality (VR) addresses these challenges directly. It moves learning beyond two-dimensional diagrams and static models, placing trainees into lifelike, three-dimensional clinical scenarios. Within this digital space, a surgical resident can perform a complex spinal fusion dozens of times, learning from each attempt without any real-world consequences.
A New Paradigm for Skill Development
This technology marks a fundamental shift from conceptual learning to applied practice. Instead of only reading about a rare cardiac condition, a medical student can virtually stand inside a beating heart to observe its function. This level of immersion fundamentally changes the educational experience.
The core benefits of integrating virtual reality into medical training are clear:
- Risk-Free Practice: Trainees can repeat procedures, familiarize themselves with instruments, and navigate simulated complications in a zero-risk environment, ensuring patient safety is never compromised.
- Enhanced Accessibility: VR democratizes high-level training. It allows institutions to offer standardized, elite instruction without the geographical or logistical constraints of specialized physical labs.
- Data-Driven Feedback: Every movement and decision within a simulation can be tracked and analyzed. This provides objective, detailed feedback on performance, pinpointing specific areas for improvement.
Virtual reality is more than an innovative technology; it is a powerful educational tool that addresses longstanding challenges in medical training. It provides a practical pathway to achieving mastery through repetition—a goal that has traditionally been difficult and costly to achieve.
Moving Beyond Traditional Limitations
By creating realistic simulations that respond to a user's actions, VR prepares medical professionals for the pressure and complexity of their roles in ways previously impossible. It closes the gap between theoretical knowledge and hands-on skill, building both competence and confidence.
The result is that trainees who engage with VR enter clinical settings better prepared, more skilled, and ready to deliver a higher standard of care from their first day.
Why Is VR Changing the Game in Medical Training?
For centuries, medical education has relied on textbooks, observation, and hands-on practice with cadavers or manikins. While effective, this system has its limits. For example, how does a surgeon practice for a once-in-a-career complication? Or how does a new clinician build confidence when their first live procedure involves a human life?
This is where VR provides a solution. It is not merely advanced technology; it is a safe, repeatable, and realistic training ground that bridges the gap between theory and practice.
Mastery Through Repetition
The primary advantage of VR is its capacity for unlimited, deliberate practice. A surgical resident can perform a complex procedure hundreds of times, facing different randomized complications with each attempt.
This is fundamentally different from reading a textbook or watching a video. It is about building muscle memory. The repetitive, hands-on nature of VR embeds procedural steps and critical decision-making deep into a learner's cognitive and motor pathways, significantly shortening the learning curve.
A New Standard for Patient Safety
This is arguably the most critical benefit. In a virtual operating room, mistakes are learning opportunities. A trainee can inadvertently damage a simulated artery, misinterpret a monitor, or select the wrong instrument—all without causing any real-world harm.
This risk-free environment is transformative. It allows medical professionals to build foundational skills and confidence simultaneously. A surgeon who has already managed a simulated arterial bleed in VR is far better equipped to handle that crisis calmly and competently in a real operating room. VR training helps prevent errors before they can reach a patient.
Simulating the Rare and the Unpredictable
Some of the most critical events a medical team will face are, fortunately, rare. Incidents such as mass casualty events or unusual surgical complications are nearly impossible to replicate for training purposes through traditional means.
VR excels at creating these high-stakes, low-frequency scenarios on demand. An entire emergency department team can run through a simulated disaster response, refining their communication and protocols in a chaotic yet controlled environment. This ensures that if a worst-case scenario occurs, the team is executing a practiced plan, not improvising for the first time. For a deeper dive, you can explore the many benefits of virtual reality training that are reshaping professional development.
Driving Efficiency and Scalability
Logistically, maintaining cadaver labs or high-fidelity physical manikins is expensive and does not scale efficiently. A VR training station, by contrast, offers a more cost-effective and flexible solution.
Once the initial hardware and software investment is made, the cost per training session is negligible. This model also overcomes geographical barriers. A training module for a world-class procedure perfected at one institution can be distributed globally, enabling organizations everywhere to deliver standardized, elite-level training.
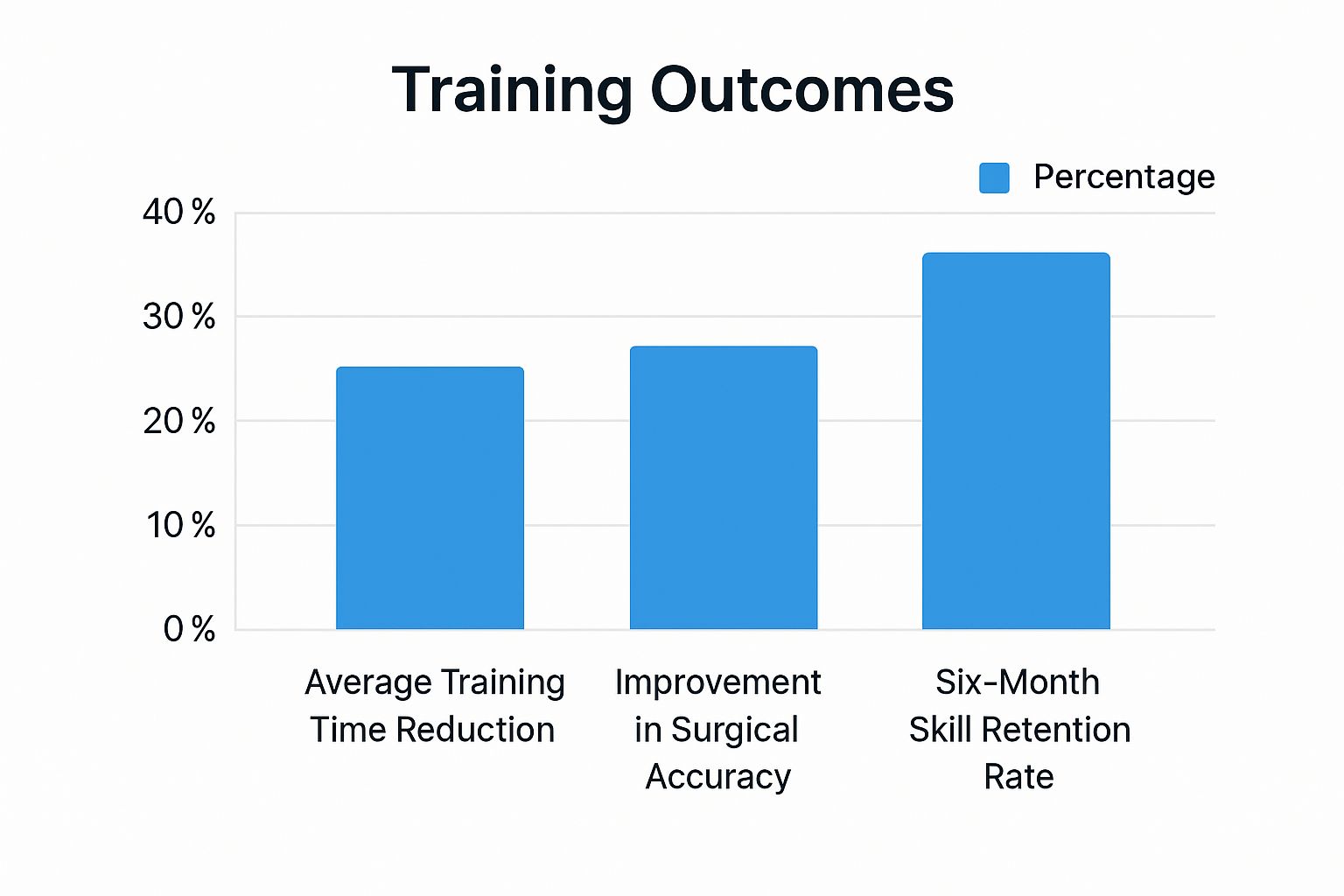
The data supports the efficacy of this approach. Studies show that VR is not just a novelty; it delivers tangible results. Surgeons trained with VR have been shown to perform up to 29% faster and make 6x fewer errors compared to their traditionally trained counterparts.
To fully appreciate the difference, it is helpful to compare the two approaches directly.
Comparing VR Training with Traditional Methods
This table outlines how VR compares to traditional methods across several key areas.
| Feature | Traditional Training (Cadavers, Manikins) | VR Training |
|---|---|---|
| Realism | High physical realism but lacks physiological response. | High procedural and environmental realism with dynamic patient responses. |
| Repetition | Limited; cadavers are single-use, and manikins require reset. | Unlimited; scenarios can be repeated instantly with variations. |
| Safety | Risk of exposure to chemicals (e.g., formaldehyde); no risk to patients. | Completely risk-free for both trainee and patient. |
| Cost | High ongoing costs for cadaver procurement, storage, and manikin maintenance. | Higher initial hardware cost, but very low cost per use. |
| Scalability | Difficult and expensive; requires physical lab space and resources. | Highly scalable; can be deployed anywhere with a headset. |
| Feedback | Dependent on instructor availability for direct observation. | Provides immediate, objective, data-driven performance feedback. |
While traditional methods remain valuable, VR offers a level of flexibility, safety, and data-driven insight that was previously unattainable. It represents a fundamental shift in how we prepare the next generation of healthcare professionals.
Real-World Applications of VR in Healthcare Education
The theoretical foundation for VR in medical training is strong, but its true value is demonstrated in real-world applications. Across a spectrum of medical fields, VR is an active tool solving tangible problems in healthcare education. From the precise environment of an operating room to the dynamic conditions of an emergency response, these immersive tools are developing safer, more competent clinicians.
VR enables trainees to experience scenarios that would be too expensive, rare, or dangerous to replicate otherwise. This hands-on experience in a digital environment is proving essential for building skills and refining decision-making under pressure.
Mastering Complex Surgical Procedures
Surgery is one of the most impactful areas for VR application. Consider a neurosurgery resident preparing for their first complex spinal fusion. Traditionally, this would involve observing senior surgeons, studying anatomical models, and perhaps practicing on a cadaver, which provides limited physiological feedback.
With virtual reality for medical training, that same resident can now perform the entire procedure dozens of times in a highly realistic simulation. They can experience haptic feedback when drilling into bone, observe how tissue responds to their instruments, and manage simulated complications like a sudden hemorrhage. This is not just about knowledge acquisition; it is about building motor skills and muscle memory.
This capability is particularly transformative in specialties that demand extreme precision and have a steep learning curve.
- Orthopedic Surgery: Trainees can practice joint replacements and fracture repairs repeatedly, perfecting their technique and alignment before entering a live surgical environment.
- Neurosurgery: Simulators allow residents to navigate the brain's delicate structures, learning to avoid critical nerves and vessels in a zero-risk setting.
- Laparoscopic Skills: VR is ideal for training the counter-intuitive motor skills required for minimally invasive surgery, tracking every movement to provide objective data on a surgeon's efficiency.
Preparing for High-Stakes Emergencies
VR also excels at preparing medical teams for rare, high-stakes emergencies that are nearly impossible to practice for. A lack of realistic training can contribute to medical errors. VR provides a safe environment for clinicians to rehearse everything from managing surgical complications to handling emergency room crises without any patient risk.
In fact, a 68% majority of physicians surveyed believe VR should be a core component of medical education. They recognize its power to provide hands-on learning without risk, allowing them to master complex cases and bridge the gap between textbook knowledge and practical skill. To learn more about physician perspectives, you can explore the full survey findings on VR in medical training.
This type of training extends beyond individual skills to team dynamics, communication, and maintaining composure under pressure.
Imagine a simulated mass casualty event where an entire emergency department team is immersed in a chaotic scene. They must work together to triage patients, manage resources, and communicate clearly under simulated stress. This provides a level of real-world preparation that a tabletop exercise cannot match.
Cultivating Empathy and Patient Communication
Effective clinical practice is not solely about technical proficiency. It also requires the ability to connect with patients, demonstrate empathy, and communicate clearly, especially during difficult conversations. VR offers a uniquely powerful way to train these "soft skills" by allowing a provider to experience a scenario from the patient's perspective.
For instance, a VR module can simulate a patient's experience receiving a difficult diagnosis. The clinician can see the environment from the hospital bed, hear the conversation from the patient's viewpoint, and even experience simulated sensory impairments.
This first-person perspective fosters a deep, genuine empathy that is difficult to cultivate through lectures alone. It helps clinicians understand how their body language, tone, and word choice are perceived by someone who is vulnerable. They can practice delivering bad news or managing anxious family members in a space where they can receive direct feedback and refine their approach. This demonstrates the broad potential of VR to improve everything from intricate surgical maneuvers to the fundamental human side of patient care.
Implementing a Successful VR Training Program
Integrating virtual reality into a medical training curriculum requires a structured, strategic plan. A successful implementation begins not with the technology, but with a clear educational strategy that aligns VR’s capabilities with specific, measurable training goals.
First, it is essential to define what you aim to achieve. Is the goal to reduce errors in a specific surgical procedure? Improve team communication during a code blue? Or accelerate the onboarding of new nurses? Establishing clear learning objectives is the foundation for an effective program.
Once your goals are defined, you can identify the skills gaps that VR is uniquely suited to address. Perhaps traditional methods are insufficient for practicing rare, high-stakes events, or junior residents require a safe space to build confidence before their first live surgery. Focusing on these areas ensures that the investment in VR will have the greatest impact.
Selecting the Right Tools for the Job
With your objectives defined, the next step is to select the appropriate hardware and software. This decision involves balancing technical capabilities with practical usability, as the ideal solution will vary between institutions.
Consider these key factors when evaluating options:
- Fidelity and Realism: Determine the necessary level of realism. A neurosurgery simulation requires photorealistic graphics and precise haptic feedback. In contrast, a module for practicing patient communication may prioritize realistic AI-driven dialogue over high-fidelity visuals.
- Usability and Scalability: Evaluate how easily the system can be used by both trainees and instructors. Standalone headsets offer simplicity and scalability, making them suitable for large-scale deployments. PC-powered VR provides greater graphical power but involves more complexity and a higher cost.
- System Integration: Ensure the VR platform can integrate with your existing Learning Management System (LMS). This allows for seamless tracking of progress and performance data alongside other training metrics, providing a holistic view of a trainee’s development.
A common mistake is to select the most advanced technology without considering the practicalities of daily use. The optimal solution is one that meets learning objectives while being user-friendly enough for faculty and students to adopt with minimal friction.
Blending Virtual and Traditional Education
VR in medical training is most effective when it supplements, rather than replaces, traditional methods. The most powerful approach is a hybrid learning model that weaves VR modules into the existing curriculum.
For example, a student might first learn the theory behind a procedure in a lecture, then use a VR simulation to practice the hands-on motor skills repeatedly. Finally, they would apply this knowledge and muscle memory in a supervised clinical setting.
This blended model creates a cohesive learning journey where each component builds on the last. It leverages the strengths of each method: foundational knowledge from lectures, safe and repetitive practice from VR, and real-world context from clinical rotations. By integrating VR in this manner, it becomes a tool that deepens understanding and accelerates the path to mastery.
Finally, a successful rollout depends on people. Ensuring faculty are comfortable and proficient with the technology is as crucial as training the students. Instructors need to know how to guide trainees through simulations, interpret performance data, and provide targeted feedback. A structured onboarding process for students helps them acclimate quickly and focus on the learning experience. Championing the technology and demonstrating its value fosters a culture of innovation.
Measuring the ROI of Your VR Training Investment
For any healthcare administrator, a primary consideration for new technology is its return on investment (ROI). While the educational benefits of virtual reality for medical training are clear, the financial case is equally compelling. Calculating the true ROI requires looking beyond initial costs to assess both direct cost savings and significant indirect gains.
The upfront investment in VR—including headsets, controllers, software licenses, and platform subscriptions—is tangible. However, these one-time costs should be weighed against the substantial, recurring expenses of traditional training methods.
Quantifying Direct Financial Savings
The most direct ROI comes from reducing or eliminating costs associated with traditional training resources. Conventional medical education relies on resource-intensive tools that carry significant price tags and logistical complexities.
VR provides a clear financial advantage by reducing dependence on:
- Cadavers and Animal Labs: The procurement, storage, and disposal of cadavers are expensive and complex. VR offers a reusable, on-demand digital alternative without recurring costs.
- Physical Simulators and Manikins: A single high-fidelity manikin can cost tens of thousands of dollars, plus ongoing maintenance and the need for dedicated simulation labs. A VR headset can run countless scenarios at a fraction of that cost.
- Travel and Facility Expenses: Since VR training can be deployed anywhere, it reduces the need to transport trainees and instructors to a central location, resulting in significant savings on flights, accommodations, and venue rentals.
The global Virtual Reality (VR) medical training market is projected to reach approximately $395.4 million by 2025 and is growing at a Compound Annual Growth Rate (CAGR) of about 15.9% between 2025 and 2033. This reflects a major industry shift toward more efficient and cost-effective training solutions.
Uncovering Significant Indirect Returns
Beyond direct savings, the indirect ROI of virtual reality for medical training often provides the most substantial long-term financial benefits. These returns stem from improved operational efficiency, reduced medical errors, and better patient outcomes.
A well-implemented VR program delivers value by lowering the costs associated with medical errors. When trainees can practice high-stakes procedures repeatedly in a risk-free environment, they enter the operating room better prepared. This leads to fewer complications and a reduced need for costly follow-up interventions.
Additionally, VR-trained professionals often demonstrate greater efficiency. They may complete procedures faster, which can lead to quicker operating room turnover and increased patient throughput. This operational improvement contributes directly to revenue and optimizes resource utilization. For a deeper analysis of this topic, refer to our guide on how to measure training effectiveness.
The Invaluable Non-Financial Gains
Finally, some of the most powerful returns from a VR investment are not easily quantifiable but are critical to an institution's long-term success. One such benefit is trainee confidence. Clinicians who have rehearsed challenging scenarios in VR are calmer and more effective when performing under pressure in a real-world setting.
Ultimately, these advantages contribute to what matters most: superior patient outcomes. Better clinical results enhance a hospital's reputation, help attract top talent, and provide a significant competitive advantage. By adopting VR, an institution is not just purchasing technology; it is positioning itself as a leader in medical innovation committed to delivering the safest and most effective care possible.
The Future of Medical Simulation Technology

The evolution of virtual reality for medical training is ongoing. Future advancements are focused on making the technology smarter, more responsive, and more collaborative, further blurring the line between simulation and reality. These developments are poised to elevate medical education to a new standard of excellence.
This next wave of innovation aims to make training less like a pre-programmed lesson and more like a dynamic, real-world clinical encounter. The focus extends beyond what trainees see to include what they feel and how they adapt to changing conditions.
Smarter Simulations With Artificial Intelligence
A significant advancement is the integration of Artificial Intelligence (AI) into VR training. Instead of static, scripted scenarios, AI creates adaptive learning environments that challenge trainees based on their real-time performance.
Imagine a virtual patient whose vital signs change dynamically in response to a trainee’s actions, creating a unique and unpredictable challenge with each simulation. This shifts the focus from simple procedural practice to honing the critical thinking and decision-making skills required in a real emergency. The future of training will likely blend immersive VR with other advanced digital tools, such as computer-based case simulations, to create a comprehensive learning ecosystem.
Haptic Feedback and Collaborative Spaces
The sense of touch is critical in medicine, and emerging haptic feedback technology is bringing this dimension into the virtual world. Future trainees will be able to:
- Feel the resistance of tissue during a virtual incision.
- Sense the subtle texture of different organs.
- Experience the tactile feedback of suturing a wound.
The addition of physical sensation builds a level of muscle memory and realism that visual-only simulations cannot replicate.
Beyond individual training, the future is collaborative. VR will enable entire surgical teams, even those in different geographical locations, to enter a shared virtual operating room. Surgeons, nurses, and anesthesiologists can practice complex procedures together, perfecting their communication and teamwork before meeting in person.
The next generation of medical VR will be defined by its intelligence and interconnectedness. It will create a global, digital training ground where skills are honed with unprecedented realism, ultimately leading to better-prepared clinicians and superior patient outcomes.
Frequently Asked Questions
Adopting any new technology naturally raises questions. We have compiled some of the most common inquiries about virtual reality in medical training to provide clear and straightforward answers.
How Does VR Training Stack Up Against Using Cadavers?
While cadavers provide an unparalleled opportunity to study real human anatomy, VR training offers several key advantages.
The most significant is the capacity for unlimited practice. A trainee can perform a complex procedure hundreds of times in VR, which is impossible with a single-use cadaver. This digital approach also eliminates the substantial costs and logistical challenges of sourcing, storing, and handling cadavers, making high-quality training more accessible.
VR also offers superior variety. With a simple selection, an instructor can introduce a wide range of patient pathologies or unexpected complications, providing trainees with a breadth of experience that is difficult to replicate through other means. While the tactile feedback of a real body is unique, VR serves as an ideal complement, offering a structured, data-driven, and completely safe environment to build and perfect procedural muscle memory.
What Kind of Gear Do I Actually Need to Get Started?
The required hardware depends on your specific training objectives. Most programs can begin with commercially available standalone VR headsets. These devices offer an effective balance of quality, cost, and ease of use suitable for a wide range of training scenarios.
For more advanced simulations, such as hyper-realistic surgical training that demands significant graphical power, a PC-powered headset connected to a high-performance computer may be necessary. For maximum immersion, some modules incorporate haptic gloves or custom controllers that mimic the feel of surgical instruments, though these are typically part of a more specialized setup.
Can VR Really Be Used to Teach Soft Skills, Like Talking to Patients?
Absolutely. VR is an exceptionally effective tool for developing the crucial soft skills that are essential for high-quality patient care. It immerses medical professionals in realistic, emotionally charged situations with AI-driven virtual patients. This allows trainees to practice difficult conversations, such as delivering bad news or de-escalating a tense situation, in a controlled environment.
A particularly powerful feature of VR is its ability to allow clinicians to see a situation from the patient’s perspective. This fosters a genuine sense of empathy that is difficult to teach in traditional role-playing exercises.
Trainees have a safe space to practice their communication style, receive immediate and objective feedback, and repeat a scenario until they achieve proficiency. This process builds the confidence and interpersonal finesse that are fundamental to patient-centered care.
Ready to see how immersive simulations can elevate your training programs? The team at AIDAR Solutions specializes in creating and integrating VR and AR solutions that deliver measurable results, from accelerating skill acquisition to improving operational efficiency. Discover how we can tailor a virtual training program for your organization at aidarsolutions.com.


