Medical Training VR: Revolutionizing Healthcare Education
Medical training in VR offers a safe, repeatable, and immersive way for healthcare professionals to practice complex procedures and develop a deep understanding of anatomy, all without patient risk.
It serves as a high-fidelity simulator for clinicians, providing critical hands-on experience that bridges the gap between textbook knowledge and real-world clinical application.
The New Standard in Medical Education

For generations, medical education has relied on methods with significant limitations. Textbooks, lectures, and observational learning can only convey so much. Meanwhile, training on cadavers or mannequins is expensive, and these resources are not always available on demand.
Critically, a resident’s first time performing a high-stakes procedure often occurs with a live patient. The pressure is immense, and the safety risks are undeniable.
This is precisely where medical training VR changes the educational paradigm. It shifts learning from passive observation to active participation. This is no longer a futuristic concept; it is an essential tool for modern healthcare institutions. By creating hyper-realistic, interactive simulations, VR technology directly addresses the core challenges that have constrained conventional training for decades.
Overcoming Traditional Training Hurdles
Virtual reality provides practical solutions to these long-standing educational roadblocks. Instead of merely reading a chapter about a rare cardiac condition, a student can now step into a virtual O.R. and manage the event in a controlled environment. This shift offers immediate, powerful advantages:
- Risk-Free Practice: Trainees can perform complex procedures hundreds of times, building the muscle memory and confidence they need without ever endangering a patient.
- Accessibility to Rare Scenarios: VR can perfectly simulate uncommon but critical medical emergencies, ensuring professionals are prepared for situations they might rarely encounter in practice.
- Standardized Learning: Every learner receives the same high-quality training experience, which ensures consistent skill development across an entire team or cohort.
This move toward immersive learning is more than a trend; it's a fundamental change in how we prepare the next generation of healthcare professionals for the complexities of their roles. It prioritizes competence and safety above all else.
The Growing Adoption of VR Training
The momentum behind this shift is undeniable, as reflected in market growth. As more institutions recognize the clear benefits, investment is increasing. The broader VR education market, heavily driven by the medical training sector, was valued at approximately $4.4 billion in 2023.
Projections show it expanding to $28.7 billion by 2030, a clear signal of its expanding role in education. You can learn more about the growth of VR in medical education and its market trends.
This growth is driven by the technology's power to create safer, more effective, and more accessible training. It gives institutions the ability to build a more skilled and confident workforce, ready to deliver top-tier patient care from day one.
How VR Forges Lifelike Clinical Worlds
Crafting a believable virtual operating room requires more than impressive graphics. The key is convincing the user's brain that they are truly present in that environment. The most effective medical training VR solutions achieve this by merging sophisticated hardware with intelligent software, turning a headset and controllers into a gateway to a high-stakes clinical scenario. This synergy elevates the experience from simply watching a video to actively participating in a hands-on learning drill.
It begins with the hardware. Modern VR headsets, such as the Meta Quest 3, boast high-resolution displays that have virtually eliminated the "screen door" effect—a distracting grid of pixels. This level of visual clarity is non-negotiable; a surgeon in training needs to see anatomical details with precision.
Combining a sharp display with a wide field of view creates a powerful sense of immersion that helps the user forget they are in a simulation. The controllers become their hands, allowing them to grip, move, and use virtual surgical tools, anatomical models, and equipment as they would in the real world.
The Game-Changer: Haptic Feedback
Sight and sound are crucial, but the sense of touch truly brings medical VR training to life. This is where haptic feedback enters the picture. It is the technology that creates tactile sensations, allowing a user to "feel" the virtual environment.
For example, when suturing tissue, there is a specific resistance and pull. Haptic technology is designed to replicate that feeling. Advanced controllers and specialized gloves can simulate the subtle buzz of a bone saw, the precise pressure needed for an incision, or the distinct feedback of a needle piercing different layers of tissue.
This tactile element is vital for building muscle memory. It closes the gap between knowing the steps of a procedure and having the hands-on skill to execute them flawlessly. Without haptics, a simulation is merely a visual walkthrough. With haptics, it becomes a genuine skill-building tool.
Assembling the Virtual World
While hardware provides the window into this new reality, software builds the world on the other side. These realistic environments are incredibly complex, relying on several layers of technology working in harmony.
- Realistic Physics Engines: These systems dictate how virtual objects interact, ensuring instruments behave as expected and that tissues react to pressure and manipulation in a medically accurate way.
- Anatomically Correct Models: The backbone of any clinical VR simulation is often found in advanced 3D medical visualization technologies, which convert static scans into living, interactive models. These are dynamic structures that can be dissected, explored, and operated on.
- Scenario-Based AI: Intelligent software directs the simulation. It can introduce unexpected complications, track user performance, and adapt the scenario in real time. An AI might, for instance, trigger a sudden drop in a patient's blood pressure, forcing the trainee to think and act under pressure.
At its core, a VR medical simulation is a finely orchestrated symphony of hardware and software. Each component works together to create a cohesive experience that is not only believable but also educationally potent.
The goal is to achieve a state of "presence," where the user’s brain fully accepts the virtual environment as real. The technology is working when a trainee’s heart rate spikes during a simulated emergency. By mimicking the sights, sounds, and feel of a real clinical setting, medical training VR provides an unmatched platform for building confidence and competence long before a trainee ever touches a real patient.
You can take a deeper look into how it all comes together in our comprehensive guide to virtual reality for medical training.
Measuring the Impact of VR on Clinical Skills
While the technology behind virtual reality is impressive, its true value in healthcare is determined by a critical question: does it create better clinicians? The evidence is clear: VR in medical training is a powerful tool for building real, measurable skills.
Hospitals and universities embracing this technology are seeing tangible improvements. Trainees not only learn procedures faster but also retain them longer. More importantly, they make significantly fewer mistakes when they step into a real clinical environment, which has a direct impact on patient safety.
From Repetition to True Competence
One of VR's greatest advantages is the freedom to practice without real-world consequences. Consider a surgical resident learning a complex cardiac procedure. Traditionally, their first few attempts occur under intense pressure, with a supervisor observing and a real patient on the table. The learning curve is steep, with no room for error.
Now, imagine that same resident using VR. They can run through the entire procedure fifty times in an afternoon. They can encounter rare complications, test different approaches, and build crucial muscle memory—all in a completely safe, simulated space. This high-volume repetition is simply not possible with traditional training methods.
This isn't just about practicing until you get it right; it's about building genuine competence. VR allows trainees to master not just the "how" but also the "why" behind every step, creating a deeper, more resilient skill set that holds up under pressure.
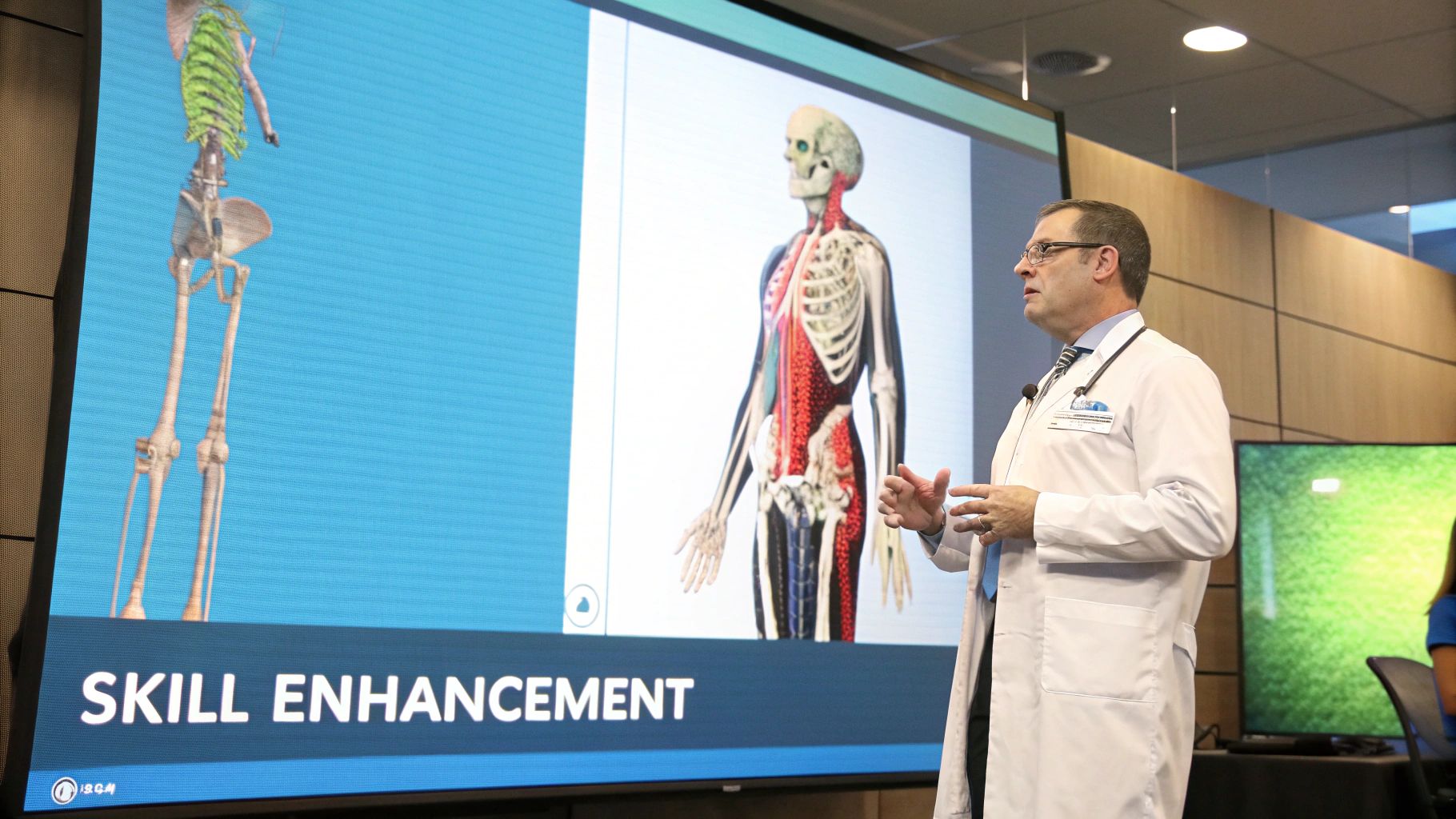
The infographic below breaks down how different types of VR medical simulations are being adopted, showing where the technology is making the biggest impact.
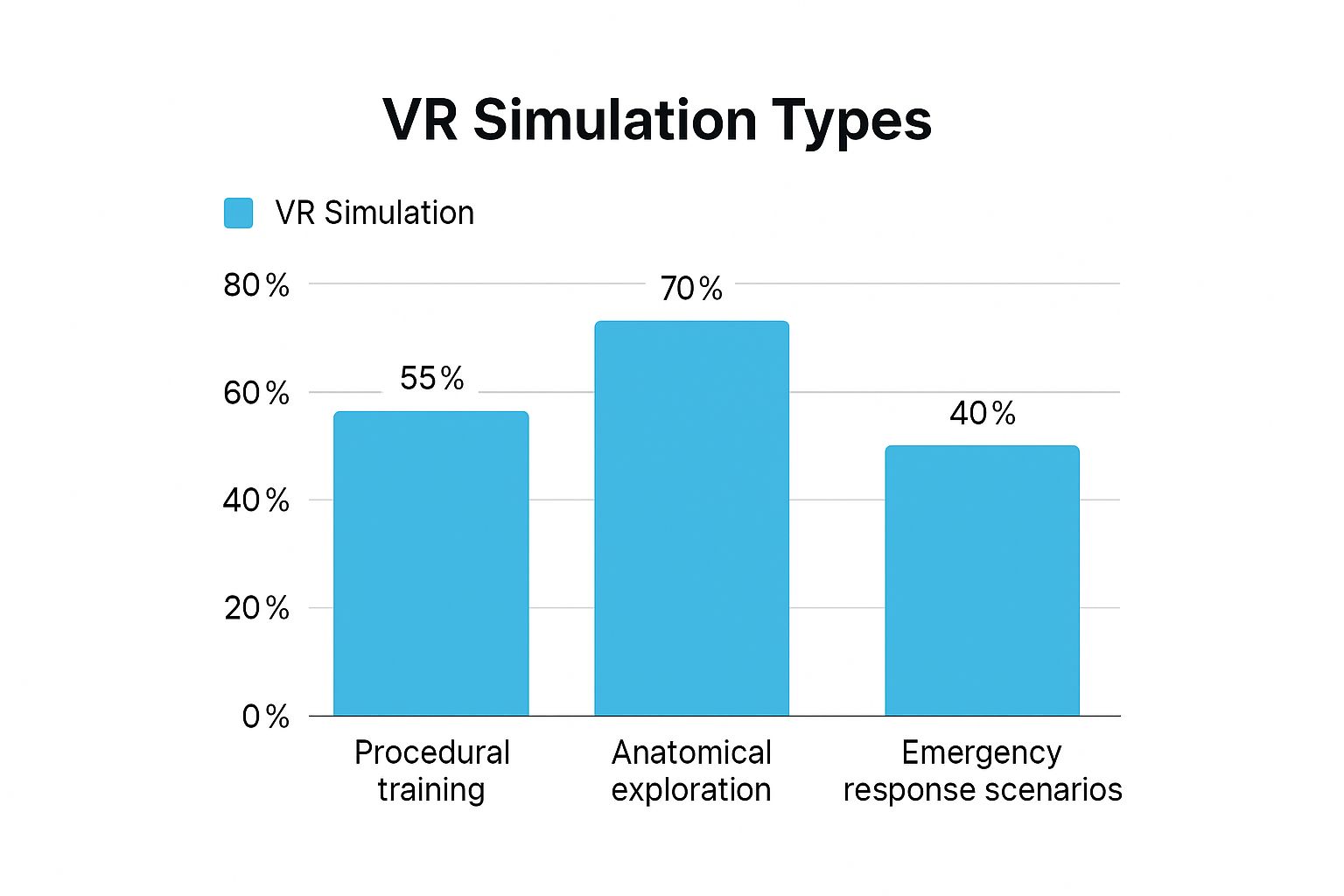
As you can see, anatomical exploration is a major use case. It perfectly highlights VR's power to help learners visualize and interact with complex biological systems in a way textbooks and diagrams never could.
The Power of Data-Driven Improvement
Beyond offering a risk-free practice zone, medical training VR delivers a level of objective performance data that was previously impossible to capture. Every movement, decision, and moment of hesitation is tracked and analyzed. This creates an incredibly detailed feedback loop for both the learner and their instructor.
This data-first approach shifts skill assessment from subjective observation to objective measurement. Key metrics often include:
- Time to Completion: How efficiently the trainee completes the procedure.
- Procedural Accuracy: The precision of their movements, such as the accuracy of an incision or the placement of a suture.
- Error Rates: Identifying and logging every deviation from the correct protocol, pointing to clear areas for improvement.
- Decision-Making Under Pressure: How trainees react when a simulated emergency or an unexpected complication is introduced.
This constant stream of feedback accelerates the learning process. To see just how effective this is, let's look at the numbers. The table below compares the outcomes from traditional training methods against those from VR simulations.
Traditional vs VR Medical Training Outcomes
| Metric | Traditional Training | VR Training |
|---|---|---|
| Skill Acquisition Speed | Slower, limited by resource availability | Up to 250% faster |
| Skill Retention (Long-Term) | Moderate, decays without practice | Up to 80% one year later |
| Procedural Error Rate | Baseline | 45% reduction |
| Trainee Confidence | Variable, often lower initially | 48% increase |
| Objective Feedback | Subjective, based on observation | Objective, data-driven |
These metrics, drawn from various clinical studies, paint a clear picture. The gains are not marginal; they represent a fundamental improvement in how we prepare our medical professionals.
Achieving Scalable, Standardized Excellence
For large hospitals and medical universities, training hundreds of students and residents to the same high standard presents a significant logistical challenge. VR resolves this issue effectively. It allows institutions to deploy a perfectly standardized curriculum to every learner, ensuring everyone receives the same quality of instruction.
This scalability means a world-class surgical simulation built at a top-tier institution can be deployed across a global network of hospitals. It levels the playing field, giving more people access to elite training and raising the overall standard of care. This is a core benefit of modern virtual reality training solutions, which are designed for this kind of broad, effective deployment. The end result is a more competent, confident, and prepared healthcare workforce, ready to tackle the challenges of modern medicine.
Practical Applications of VR in Healthcare Training
The power of VR in medical training extends far beyond the operating room. While surgical simulation is a prominent application, the technology's true strength lies in its versatility. It is solving practical training challenges across the healthcare spectrum, from foundational anatomy lessons to the delicate art of patient communication.
Instead of memorizing diagrams from a textbook, medical students can now take a guided tour inside a living, beating heart, watching valves open and close in real time. This shift from two-dimensional learning to immersive, three-dimensional exploration builds a deeper, more intuitive understanding that is retained more effectively.
Interactive Anatomy and Physiology Labs
One of the most immediate and powerful uses for VR is teaching anatomy. Traditional methods, like working with cadavers, are constrained by high costs, limited availability, and the fact that they only offer a static, non-living view of the human body. VR completely changes this dynamic.
Inside a virtual anatomy lab, a student can:
- Isolate Organ Systems: Instantly fade out the skeletal system to get a perfectly clear view of the entire circulatory network.
- Explore at a Cellular Level: Shrink down to the size of a microbe and watch blood cells flow through an artery.
- Manipulate Structures: Pick up a virtual brain, rotate it, and disassemble it piece by piece to see how intricate parts fit together.
This hands-on, interactive approach makes a difficult subject engaging and memorable. It builds the solid foundational knowledge that is critical for all future clinical work.
Refining Patient Communication and Empathy
A clinician's skill is measured not only by clinical expertise but also by their ability to communicate with patients. Practicing these difficult conversations has always been a challenge. Using actors for role-playing is expensive and hard to scale, which often leaves new doctors unprepared for the emotional weight of breaking bad news or calming a distressed family member.
VR creates a scalable and emotionally safe space to build these crucial "soft skills." Trainees can interact with AI-driven virtual humans and practice a wide range of scenarios. These virtual patients react realistically—showing frustration, confusion, or relief based on the trainee's words and tone. This allows clinicians to rehearse high-stakes conversations repeatedly until they feel confident and prepared.
By simulating the human side of medicine, VR helps develop the empathy and communication skills that are as vital as procedural know-how. It prepares clinicians for the real and often difficult emotional landscape of patient care.
The rapid adoption of these varied applications is a key reason the global Virtual Reality (VR) medical training market is growing so quickly. It's projected to reach an estimated value of $395.4 million by 2025 and is expected to grow at a rate of nearly 16% annually through 2033, driven by these diverse and effective use cases.
High-Stakes Emergency Response Drills
In a chaotic emergency room, teamwork and clear communication can be the difference between life and death. Recreating the intense pressure of a mass casualty event or a complex trauma case for training is nearly impossible in the real world. VR simulations, however, can replicate it with high fidelity.
Multi-user VR platforms allow entire medical teams—doctors, nurses, and technicians—to step into a shared virtual space and work through a crisis together. They must communicate clearly, delegate tasks, and make split-second decisions as the scenario intensifies. This type of training is invaluable for improving team cohesion and identifying process breakdowns before they can occur during a real emergency.
The opportunity to practice these skills is one of the most powerful benefits of virtual reality training in any high-pressure field. By turning abstract protocols into a lived, felt experience, VR prepares healthcare teams to perform at their best when it matters most.
How to Bring a VR Training Program to Life

Implementing a medical VR training program is a strategic initiative, not just a technology purchase. A solid plan is required to ensure the investment leads to better clinical skills and patient outcomes. A thoughtful, phased approach helps avoid common pitfalls and builds a sustainable program.
The process begins long before any hardware is unboxed. It starts with a critical question: What specific training problem are we trying to solve? Without a clear answer, even the most advanced technology will fail to deliver results.
Nail Down Your Learning Objectives
Before considering hardware or software, you must pinpoint your goals. Are you aiming to reduce errors in a particular surgical procedure? Help first-year students grasp complex anatomy? Or sharpen teamwork during emergency drills? Clear objectives will guide your entire implementation.
These goals must be specific, measurable, and tied directly to curricular needs. For example, a strong objective would be: "Reduce the time required for residents to achieve proficiency in laparoscopic suturing by 30% within six months." This clarity makes subsequent decisions much easier.
Start Small With a Pilot Program
Attempting a massive, institution-wide deployment from the start is often a recipe for failure, as it can overwhelm teams and budgets. A more effective approach is to begin with a focused pilot program. This allows you to test the technology on a smaller scale, gather invaluable feedback, and build a solid case for expansion.
Select a single department or even a single course for your pilot. This controlled setting makes it easier to manage the technical setup, train a small group of instructors, and closely monitor the results. The objective is to prove the concept and demonstrate its value quickly.
A successful pilot program does more than just validate the technology; it creates internal champions. When other departments see the positive impact on a small group of trainees, they become advocates for expansion, making the transition much smoother.
Pick the Right Hardware and Software
With your objectives defined, you can now select the right tools for the job. The VR hardware market ranges from accessible standalone headsets to high-fidelity, PC-powered systems designed for complex simulations. Your choice must align with the demands of your training modules.
The software is equally crucial. You must decide whether to use off-the-shelf training applications or develop a custom-built simulation to meet a unique learning goal. Evaluate platforms based on their clinical accuracy, ease of use, and—most importantly—their data and analytics capabilities.
Effective programs provide detailed feedback on user performance. Look for solutions that track key metrics such as:
- Completion Time: How long it takes a learner to complete a task.
- Procedural Accuracy: The precision of their movements and adherence to protocol.
- Decision-Making Pathways: The choices a trainee makes during a scenario.
This data is the foundation of real skill improvement. For a deeper dive, check out our guide on how to measure training effectiveness.
Integrate and Scale With Care
Once your pilot has proven successful, you can begin planning a wider rollout. This phase is about weaving VR training seamlessly into your existing curriculum. VR modules should not feel like a separate activity; they should be a natural extension of lectures, hands-on labs, and clinical rotations.
Prepare your infrastructure for the increased demand. This means ensuring you have adequate physical space for VR stations and a strong IT support team to handle setup and troubleshooting. Most importantly, invest in robust training for your faculty. They must be comfortable with the technology to guide learners effectively and interpret performance data.
By following this structured path, you can successfully implement a medical training VR program that delivers consistent, measurable results and prepares the next generation of healthcare professionals for the challenges ahead.
The Future of Immersive Healthcare Education
The journey of VR in medical training is just beginning. Today's simulations are already creating more competent and confident clinicians. However, the next wave of advancements promises an even deeper, more intelligent learning experience. This evolution is not just about better graphics—it's about creating truly dynamic and responsive educational worlds.
At the forefront of this evolution is the integration of Artificial Intelligence. Imagine a simulation that does more than guide a user through a pre-programmed scenario. With AI, a virtual patient’s condition could evolve unpredictably based on the trainee’s actions, forcing them to think on their feet and adapt in real time, just as in a real clinical setting.
The Rise of Adaptive Learning
The most significant shift is the move toward personalized, adaptive training. An AI-powered system can monitor a learner's performance in real time, identifying subtle hesitations or recurring mistakes. It can then dynamically adjust the difficulty, introduce new complications, or offer targeted feedback to address specific weaknesses.
This creates a bespoke learning path for every user. Instead of a one-size-fits-all module, the simulation becomes a personal mentor that pushes each trainee to the edge of their capabilities, maximizing the speed and effectiveness of their learning. Looking ahead, we will see more VR simulations integrated with other advanced technologies, such as AI voice recognition in healthcare, to create even more comprehensive and realistic training scenarios.
The core message is clear: VR is fundamentally reshaping medical education. It’s creating a new foundation for medical excellence by producing a more prepared, skilled, and confident healthcare workforce.
The Next Frontier in Realism
In addition to the AI revolution, advancements in haptic technology are poised to make these experiences far more tangible. Future developments promise a much higher degree of tactile realism, allowing users to feel the subtle differences between various tissue types or the precise feedback from a delicate instrument. This heightened sensory input will further blur the line between simulation and reality, making the transition to the operating room even smoother.
Ultimately, medical training VR is moving beyond being a supplemental tool. It is becoming an essential pillar of modern medical education. By combining immersive visuals with intelligent feedback and realistic tactile sensations, this technology is not just changing how we train our healthcare professionals—it's elevating the standard of care for generations to come.
Common Questions About Medical VR Training
When institutions begin exploring immersive technology, several practical questions consistently arise. Understanding the effectiveness, cost, and equipment requirements is the first step toward making an informed decision about integrating VR into your curriculum.
Let's address some of the most common questions.
Is VR Medical Training Actually Better Than the Old Way?
The data is clear: VR training is highly effective, and in many cases, it produces superior results. Research shows that trainees using VR can reduce their procedural error rates by up to 45% and emerge with significantly greater confidence. This is not about replacing instructors; it is about empowering them with a powerful new tool.
The primary advantage lies in the ability to practice procedures repeatedly in a safe, standardized setting. This allows learners to build muscle memory and sharpen their decision-making skills at their own pace—without ever putting a real patient at risk. That is an outcome a textbook simply cannot achieve.
What’s the Real Cost to Get a VR Training Program Started?
The initial investment can vary widely depending on your objectives. A program can start small with a few affordable standalone VR headsets, which is an excellent way to run a pilot program or equip a single department. However, high-fidelity surgical simulations will require high-end, PC-powered headsets and specialized haptic equipment, which increases the cost.
It is important to consider the long-term return on investment.
Over time, VR can dramatically reduce expenditures on cadavers, animal labs, and expensive training mannequins. A common and effective approach is to start with a focused pilot program. This keeps initial costs manageable and allows you to prove the concept before committing to a larger-scale implementation.
So, Can VR Just Replace Traditional Medical School?
No, nor is it designed to. Medical VR should be viewed as a powerful supplement, not a replacement. Its function is to enrich the curriculum and address gaps that traditional methods have historically struggled to fill.
While VR is excellent for practicing specific procedures and understanding complex 3D anatomy, it cannot replicate the invaluable experiences of real-world medicine, such as:
- Real-life Patient Interaction: The subtle art of communicating with and treating actual human beings.
- Clinical Teamwork Dynamics: The unscripted collaboration that occurs in a busy clinic or ER.
- Expert Mentorship: The direct, irreplaceable wisdom gained from an experienced physician.
The most effective programs use a blended approach, mixing VR simulations with traditional lectures, hands-on workshops, and supervised clinical practice. This creates a more well-rounded and robust learning experience, preparing clinicians for all aspects of their demanding profession.
At AIDAR Solutions, we specialize in creating immersive VR training that builds more skilled and confident healthcare teams. See how our platforms can elevate your educational outcomes by visiting https://aidarsolutions.com.


